Illustration of antibodies. Credit: Shutterstock
Antibody protection against harmful forms of fungi in the gut may be disrupted in some patients with Crohn’s disease—a condition caused by chronic inflammation in the bowel—according to a new study by Weill Cornell Medicine investigators.
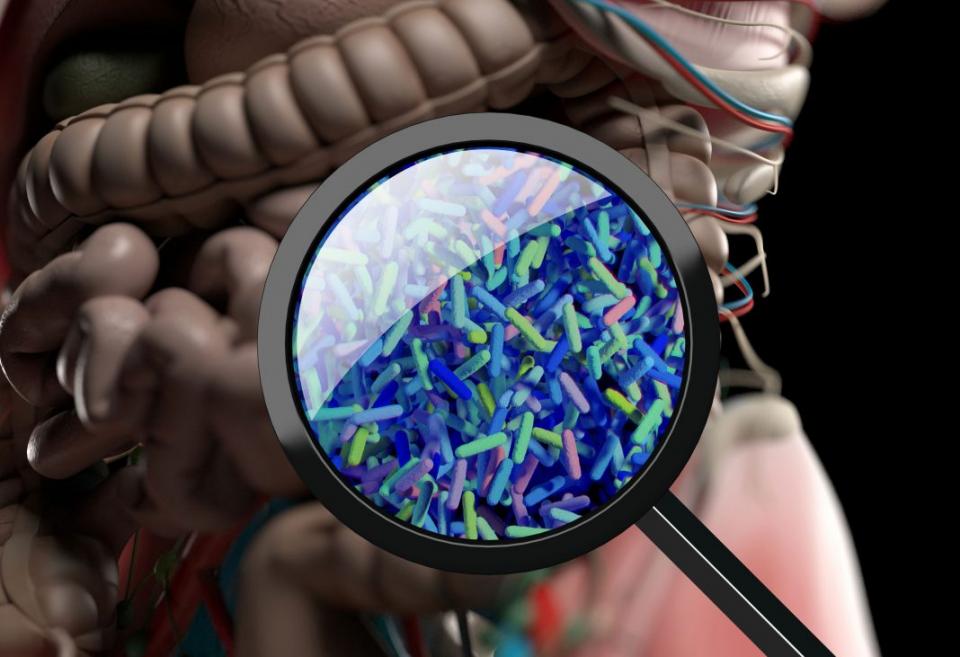
Previous studies have shown that the immune system plays a key role in maintaining a healthy balance of gut bacteria. In the new study, published Nov. 22 in Nature Microbiology, senior author Dr. Iliyan Iliev, associate professor of immunology in medicine in the Division of Gastroenterology and Hepatology, and his team at Weill Cornell Medicine investigated if it might also play a role in managing gut fungi. Unlike bacteria, fungi can change their shape in response to environmental conditions, and certain forms are harmful to humans. In particular, a type of fungus called Candida albicans transforms from a yeast form that is not pathogenic to a form that produces long, branched structures called hyphae, which can invade tissues and cause damage.

(From left) Dr. Iliyan Iliev and Itai Doron.
The investigators found that antibodies that are secreted in the gut help control the pathogenesis of Candida albicans in healthy individuals and that this protective mechanism may be disabled in people with Crohn’s disease, causing a harmful overgrowth of the pathogenic form of the fungus. An intestinal overabundance of Candida albicans is associated with inflammatory bowel disease and several other conditions that directly or indirectly affect the gastrointestinal tract.
“We found that antibodies secreted in the gut are involved in maintaining specific intestinal fungi such as C. albicans in its benign, so-called commensal form,” said Dr. Iliev, who is also a scientist in the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine. “This process is interrupted in patients with Crohn’s disease.” To read more, click here.