Fungi in the healthy gut stimulate production of antibodies against more pathogenic species, such as Candida albicans and Candida auris (above), major causes of fungal disease in immunosuppressed patients and the elderly. Image credit: Stephanie Rossow, CDC
Common fungi, often present in the gut, teach the immune system how to respond to their more dangerous relatives, according to new research from scientists at Weill Cornell Medicine. Breakdowns in this process can leave people susceptible to deadly fungal infections.
The study, published Feb. 5 in Cell, reveals a new twist in the complex relationship between humans and their associated microbes, and points the way toward novel therapies that could help combat a rising tide of drug-resistant pathogens.

Dr. Iliyan Iliev
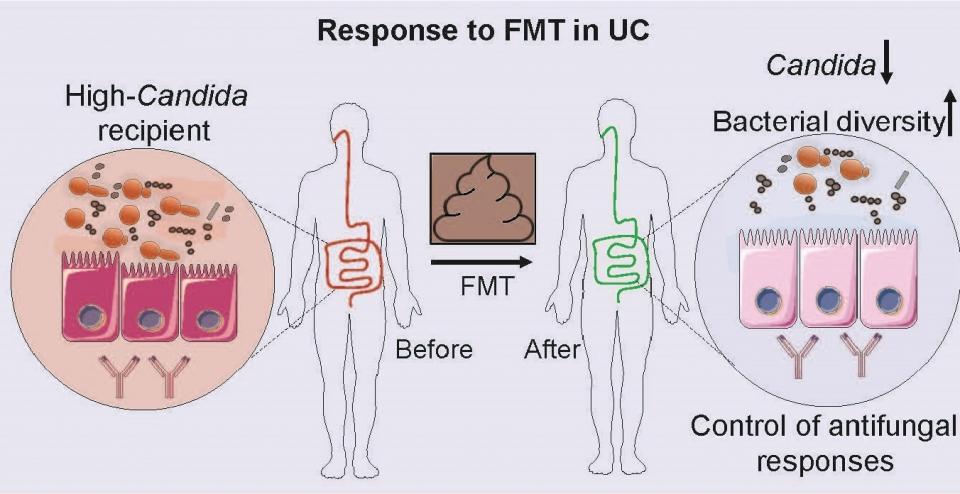
The new discovery stemmed from work on inflammatory bowel disease, which often causes patients to carry larger than normal populations of fungi in their guts. These patients often develop strong antibody responses against mannan, a molecule common to a wide range of fungal species. However, Dr. Iliyan Iliev, associate professor of immunology in medicine in the Division of Gastroenterology and Hepatology at Weill Cornell Medicine, noticed that healthy controls in these studies also had some level of anti-fungal antibodies. "There was no actual evidence for fungal infections in the healthy individuals that we examined, so we started thinking about the possible function of those antibodies," said Dr. Iliev, who is senior author on the study and a member of the Jill Roberts Institute for Research in Inflammatory Bowel Disease.
The team developed a platform that allowed them to determine which gut fungi are targeted by antibodies in the blood of individual patients. They detected a strong response against the yeast Candida albicans. Turning to experiments in mice, Dr. Iliev and Itai Doron, a Weill Cornell Medicine Graduate School of Medical Sciences doctoral candidate in the lab and lead author on the study, found that colonizing the animals' guts with Candida albicans caused them to develop antibodies against the fungus in their bloodstreams, even though they didn't develop blood-borne fungal infections. Instead, the animals' immune cells appeared to transport fungal antigens to the spleen, stimulating the production of circulating antibodies in the bloodstream. "Those fungi just educate that immune response," Dr. Iliev said.
Itai Doron
In patients with suppressed immune systems, such as organ transplant recipients and some cancer patients, fungi in the gut can invade the bloodstream and cause life-threatening infections. Dr. Iliev and his colleagues mimicked this process by treating mice with immunosuppressive drugs. When a Candida species colonizes the gut of these mice, the fungus moves into the bloodstream, causing a fatal infection. Treating the mice with purified anti-fungal antibodies from donor animals protected the immunosuppressed mice from these infections. The same strategy worked against infection with either Candida albicans or the emerging pathogenic yeast Candida auris, which has become a major cause of fungal disease in immunosuppressed patients and the elderly in recent years. To read more, click here.